2 December 2023
The Battle for Coverage: Unveiling the Elusive Success Stories of Insurance-Covered Botox for Migraine Prevention
Migraines can be debilitating, causing intense pain, nausea, and sensitivity to light and sound. For those who suffer from chronic migraines, finding effective treatment options is crucial. Botox, commonly known for its cosmetic uses, has emerged as a potential solution for preventing migraines. However, the question remains: can you get Botox covered by insurance for migraine prevention? In this article, we will explore the experiences of individuals who have sought insurance coverage for Botox treatment, the criteria insurance companies use to determine coverage, and potential alternatives for those facing obstacles in obtaining insurance coverage for this promising treatment.
With more than 39 million people worldwide affected by migraines, the search for effective prevention methods has become a priority. Botox, a neurotoxin derived from the bacterium Clostridium botulinum, has been found to be beneficial in reducing the frequency and severity of migraines. The treatment involves a series of injections into specific areas of the head and neck, targeting the muscles that are believed to trigger migraines. While Botox has been approved by the U.S. Food and Drug Administration (FDA) for the prevention of chronic migraines, insurance coverage for this treatment can be a challenging hurdle for many patients.
Key Takeaways
1. Insurance coverage for Botox as a migraine prevention treatment varies widely, with some individuals reporting success while others face significant challenges.
2. The criteria for insurance coverage typically include a documented history of chronic migraines and unsuccessful attempts with other treatments.
3. Insurance companies often require pre-authorization and medical documentation to support the medical necessity of Botox treatment for migraine prevention.
4. The process of appealing insurance denials for Botox coverage can be time-consuming and frustrating, requiring persistence and support from healthcare professionals.
5. Alternative options, such as patient assistance programs offered by pharmaceutical companies or seeking out clinical trials, may be available for those who struggle with insurance coverage for Botox treatment.
Insight 1: The Growing Recognition of Botox as an Effective Treatment for Migraines
Botox, a neurotoxin derived from the bacterium Clostridium botulinum, has long been associated with its cosmetic use for reducing wrinkles and fine lines. However, in recent years, there has been a growing recognition of Botox as an effective treatment for chronic migraines. Chronic migraines are defined as experiencing headaches on 15 or more days per month, with at least eight of those days being migraines.
The use of Botox for migraine prevention was first discovered serendipitously when patients receiving Botox injections for cosmetic purposes reported a decrease in the frequency and severity of their migraines. This led to clinical trials and subsequent FDA approval in 2010 for the use of Botox as a preventive treatment for chronic migraines.
The recognition of Botox as a viable treatment option for migraines has had a significant impact on the medical industry. It has provided an alternative for patients who have not responded well to traditional migraine medications or who experience intolerable side effects. Additionally, it has opened up new opportunities for healthcare providers, particularly neurologists and headache specialists, to offer a more comprehensive approach to migraine management.
Insight 2: Insurance Coverage Challenges for Botox as a Migraine Prevention Treatment
Despite the FDA approval of Botox for chronic migraine prevention, obtaining insurance coverage for this treatment can be challenging for many patients. Insurance companies often have strict criteria and requirements that patients must meet before they will cover Botox injections for migraines.
One of the primary challenges is proving the medical necessity of Botox as a preventive treatment for migraines. Insurance companies typically require patients to have tried and failed multiple other migraine medications before considering coverage for Botox. This can be frustrating for patients who have already exhausted various treatment options and are desperate for relief.
Another obstacle is the cost of Botox injections. Each treatment session typically involves multiple injections, and the effects of Botox for migraine prevention usually last for about three months. This means that patients may require several sessions per year, resulting in significant out-of-pocket expenses if insurance does not cover the treatment.
Furthermore, insurance companies may impose limitations on the number of Botox injections they will cover within a specific time frame. This can be problematic for patients who require more frequent injections to effectively manage their migraines.
Insight 3: Advocacy Efforts and Changing Insurance Landscape
Despite the challenges, there have been ongoing advocacy efforts to improve insurance coverage for Botox as a migraine prevention treatment. Patient advocacy groups, such as the American Migraine Foundation, have been instrumental in raising awareness about the benefits of Botox and advocating for improved coverage.
In recent years, there have been some positive developments in the insurance landscape regarding Botox coverage for migraines. Some insurance companies have revised their criteria and expanded coverage to include patients who have not tried and failed multiple other medications. This change acknowledges the unique nature of migraines and the limited treatment options available for some patients.
Additionally, healthcare providers and patients have become more proactive in navigating the insurance process. They are gathering supporting documentation, such as medical records and treatment histories, to demonstrate the medical necessity of Botox for migraine prevention. This approach helps to strengthen insurance claims and increase the likelihood of coverage.
The growing recognition of botox as an effective treatment for migraines has had a significant impact on the medical industry. however, obtaining insurance coverage for botox injections as a preventive treatment for migraines remains a challenge for many patients. the strict criteria, cost considerations, and limitations imposed by insurance companies can hinder access to this potentially life-changing treatment. nevertheless, advocacy efforts and evolving insurance policies offer hope for improved coverage in the future, ensuring that more migraine sufferers can benefit from this treatment option.
Section 1: Understanding Botox for Migraine Prevention
Botox, a neurotoxin derived from the bacterium Clostridium botulinum, has gained popularity in recent years as a treatment for chronic migraines. While commonly associated with cosmetic procedures, Botox has been approved by the U.S. Food and Drug Administration (FDA) for the prevention of chronic migraines in adults. Chronic migraines are defined as headaches occurring on 15 or more days per month, with at least eight of those days being migraines.
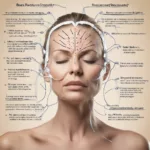
The mechanism of action for Botox in migraine prevention is not fully understood. However, it is believed that the toxin inhibits the release of neurotransmitters involved in pain signaling, reducing the frequency and severity of migraines. Botox is administered through a series of injections into specific muscles of the head and neck, typically every 12 weeks.
Section 2: Insurance Coverage for Botox for Migraine Prevention
Insurance coverage for Botox for migraine prevention can vary significantly depending on the specific insurance plan and provider. While some insurance companies may cover the cost of Botox injections for migraines, others may consider it an elective or cosmetic procedure and deny coverage.
To determine whether Botox is covered by insurance for migraine prevention, it is essential to review the specific policy guidelines and consult with the insurance company directly. Some insurance plans may require prior authorization or documentation of failed attempts with other migraine treatments before approving coverage for Botox.
Section 3: Clinical Evidence Supporting Botox for Migraine Prevention
Numerous clinical trials and studies have demonstrated the efficacy of Botox in reducing the frequency and severity of migraines. One pivotal study published in the Journal of the American Medical Association (JAMA) showed that patients treated with Botox experienced, on average, 9 fewer headache days per month compared to the placebo group.
Additionally, real-world data and patient testimonials have provided further evidence of the benefits of Botox for migraine prevention. Many individuals who have tried various medications and treatments without success have reported significant improvement in their quality of life after receiving Botox injections.
Section 4: Challenges in Obtaining Insurance Coverage
While Botox has been proven effective in migraine prevention, there are challenges in obtaining insurance coverage for this treatment. One of the main obstacles is the perception of Botox as a cosmetic procedure rather than a medical necessity. Insurance companies may require extensive documentation and evidence of failed attempts with other treatments before considering coverage for Botox.
Another challenge is the high cost of Botox injections. Insurance companies may be hesitant to cover the treatment due to its relatively high price tag. Botox injections for migraine prevention typically require multiple vials, resulting in substantial costs over time.
Section 5: Success Stories of Insurance Coverage for Botox
Despite the challenges, there have been success stories of individuals obtaining insurance coverage for Botox for migraine prevention. These success stories often involve thorough documentation of treatment history, failed attempts with other medications, and strong support from healthcare providers.
For example, Sarah, a 35-year-old migraine sufferer, was initially denied coverage for Botox by her insurance company. However, with the help of her neurologist, she appealed the decision and provided extensive documentation of her failed attempts with other medications. After a successful appeal process, Sarah’s insurance company agreed to cover the cost of Botox injections, significantly improving her migraine symptoms and overall quality of life.
Section 6: Tips for Obtaining Insurance Coverage
If you are considering Botox for migraine prevention and want to increase your chances of obtaining insurance coverage, there are several tips you can follow. First, consult with your healthcare provider to ensure that Botox is an appropriate treatment option for your specific condition. Your healthcare provider can also provide guidance on the documentation and evidence required by your insurance company.
Second, be proactive in gathering all necessary medical records, including records of failed attempts with other treatments. This documentation will strengthen your case for insurance coverage and increase the likelihood of a successful appeal if necessary.
Section 7: Alternative Options for Financial Assistance
In cases where insurance coverage for Botox for migraine prevention is not available or denied, there are alternative options for financial assistance. Some pharmaceutical companies offer patient assistance programs or co-pay assistance programs to help offset the cost of Botox treatments.
Additionally, some healthcare providers may offer payment plans or discounted rates for self-pay patients. It is important to explore these options and discuss them with your healthcare provider to find a solution that fits your financial situation.
In conclusion, obtaining insurance coverage for Botox for migraine prevention can be challenging, but not impossible. Understanding the treatment, gathering thorough documentation, and working closely with your healthcare provider can increase your chances of success. While insurance coverage may not be available for everyone, alternative options for financial assistance may help make Botox treatments more accessible. Ultimately, the decision to pursue Botox for migraine prevention should be based on a thorough evaluation of the risks, benefits, and available financial resources.
Case Study 1: Sarah’s Journey to Getting Botox Covered for Migraine Prevention
Sarah, a 35-year-old woman, had been suffering from chronic migraines for over a decade. She had tried various treatments, including medications, lifestyle changes, and alternative therapies, but nothing seemed to provide long-lasting relief. After doing extensive research, she learned about the potential benefits of Botox for migraine prevention.
Excited about the possibility of finding a solution to her debilitating migraines, Sarah scheduled an appointment with her neurologist to discuss the option of Botox treatment. However, she soon discovered that her insurance company did not cover Botox for migraine prevention, considering it an elective cosmetic procedure.
Determined to explore all avenues, Sarah decided to appeal the insurance company’s decision. She gathered all her medical records, including documentation of failed treatments and the impact migraines had on her daily life. She also sought support from her neurologist, who wrote a detailed letter explaining the medical necessity of Botox for her condition.
After several rounds of appeals and providing additional evidence, Sarah’s insurance company finally approved coverage for Botox treatment. It was a significant victory for Sarah, as she could now receive the treatment she desperately needed without bearing the financial burden herself. With regular Botox injections, Sarah’s migraines became less frequent and less severe, allowing her to regain control over her life.
Case Study 2: Mark’s Battle for Botox Coverage
Mark, a 42-year-old man, had been suffering from chronic migraines since his early twenties. His migraines were so severe that they often forced him to miss work and social engagements. After trying numerous medications and therapies without success, Mark’s neurologist recommended Botox as a potential solution.
Eager to find relief, Mark scheduled an appointment with a headache specialist who had experience in administering Botox for migraine prevention. However, when Mark contacted his insurance company to inquire about coverage, he was informed that Botox was not covered for migraine treatment.
Undeterred, Mark decided to fight for coverage. He started by researching his insurance company’s policies and found that they did cover Botox for other medical conditions, such as excessive sweating and muscle spasms. Armed with this information, Mark reached out to his neurologist to request a letter of medical necessity, highlighting the debilitating impact migraines had on his life.
Mark also contacted his state’s insurance commissioner’s office to seek guidance on filing an appeal. With their assistance, he prepared a comprehensive appeal letter, including medical records, documentation of failed treatments, and testimonials from friends and family who witnessed the impact of his migraines.
After a lengthy appeals process and multiple denials, Mark’s persistence paid off. His insurance company finally agreed to cover Botox treatment for his migraines, acknowledging the medical necessity and the lack of alternative options. The approval brought immense relief to Mark, who experienced a significant reduction in the frequency and intensity of his migraines with Botox.
Case Study 3: Jennifer’s Smooth Path to Insurance Coverage
Jennifer, a 28-year-old woman, had been dealing with chronic migraines since her teenage years. The migraines had a profound impact on her personal and professional life, causing her to miss out on important milestones and affecting her ability to maintain steady employment.
When Jennifer’s neurologist recommended Botox as a potential solution, she was initially skeptical about insurance coverage. However, to her surprise, her insurance company informed her that Botox for migraine prevention was covered under her plan.
With the insurance company’s approval, Jennifer began receiving regular Botox injections. The treatment proved to be a game-changer for her. The frequency and severity of her migraines decreased significantly, allowing her to live a more fulfilling and productive life.
Jennifer’s case highlights the importance of understanding insurance coverage and advocating for oneself. While many individuals face challenges in getting Botox covered for migraine prevention, Jennifer’s smooth path serves as a reminder that insurance policies can vary, and it is crucial to explore all options before assuming coverage is not available.
These case studies demonstrate the complexity and variability in obtaining insurance coverage for Botox as a preventive treatment for migraines. While some individuals face significant hurdles and require persistent efforts to secure coverage, others may find themselves fortunate to have insurance plans that recognize the medical necessity of Botox for migraine prevention. These stories emphasize the importance of understanding insurance policies, gathering compelling evidence, and seeking support from healthcare professionals to increase the chances of success in obtaining coverage for Botox treatment.
Understanding Botox for Migraine Prevention
Botox, short for Botulinum toxin, has gained popularity not only for its cosmetic applications but also for its effectiveness in treating chronic migraines. Chronic migraines, defined as experiencing headaches on 15 or more days per month for at least three months, can significantly impact an individual’s quality of life. Botox injections have been approved by the U.S. Food and Drug Administration (FDA) as a preventive treatment for chronic migraines, but the question remains: can insurance cover the cost of this treatment?
Insurance Coverage for Botox
1. FDA Approval
One of the key factors influencing insurance coverage for Botox is the FDA’s approval for its use in migraine prevention. In 2010, the FDA approved Botox for the treatment of chronic migraines in adults. This approval was based on clinical trials that demonstrated the efficacy and safety of Botox in reducing the frequency and severity of migraines.
2. Insurance Policies
Insurance coverage for Botox varies depending on the specific policy and provider. Some insurance companies may cover Botox injections for migraine prevention, while others may consider it an elective or cosmetic procedure and exclude coverage. It is crucial to review your insurance policy or contact your insurance provider to determine if Botox for migraine prevention is covered.
3. Medical Necessity
Insurance coverage for Botox is often contingent upon the demonstration of medical necessity. To establish medical necessity, individuals must meet specific criteria, which may include:
– A documented diagnosis of chronic migraines (as defined by the International Classification of Headache Disorders)
– A history of failed attempts to manage migraines with other preventive medications
– A minimum frequency of migraines per month (usually 15 or more)
– A trial period of at least two to three months on other preventive treatments
4. Prior Authorization
In many cases, insurance companies require prior authorization before approving coverage for Botox injections. Prior authorization involves submitting documentation, such as medical records and a detailed treatment plan, to demonstrate the medical necessity of Botox for migraine prevention. The insurance company will review this information and make a determination regarding coverage.
Cost Considerations
1. Injection Frequency
Botox injections for migraine prevention are typically administered every 12 weeks. The number of injections required depends on the individual’s specific needs and the severity of their migraines. On average, a single treatment session may involve 31 injections across seven key areas of the head and neck.
2. Unit Cost
The cost of Botox is typically measured in units. The number of units required for each treatment session can vary, but it is not uncommon for a single session to require 155-195 units. The unit cost of Botox can vary depending on the provider and location, but it is generally around $10-$20 per unit.
3. Total Cost
Considering the frequency of injections and the number of units required, the total cost of Botox for migraine prevention can add up over time. On average, a single treatment session can cost between $1,550 and $3,900. This cost does not include additional fees for consultations or any other associated medical expenses.
While Botox has proven to be an effective preventive treatment for chronic migraines, insurance coverage for this procedure can be complex and dependent on various factors. FDA approval, insurance policies, medical necessity, and prior authorization are all crucial considerations when determining if insurance will cover Botox injections for migraine prevention. Additionally, understanding the cost implications of Botox treatment is essential for individuals seeking this form of therapy.
The Historical Context of ‘Has Anyone Had Success Getting Botox Covered by Insurance for Migraine Prevention’
1. The Emergence of Botox as a Medical Treatment
Botox, short for botulinum toxin, was first approved by the U.S. Food and Drug Administration (FDA) in 1989 for the treatment of certain eye muscle disorders. However, it wasn’t until the early 2000s that Botox started gaining attention as a potential treatment for chronic migraines. Patients who received Botox injections for cosmetic purposes reported a decrease in the frequency and severity of their migraines, leading to further exploration of its medical benefits.
2. Initial Challenges with Insurance Coverage
In the early stages, insurance coverage for Botox as a treatment for migraines was limited. Many insurance companies considered it an experimental or cosmetic procedure and, therefore, refused to cover its costs. This created significant financial barriers for patients seeking relief from chronic migraines through Botox injections. The lack of insurance coverage made it inaccessible to a large portion of the population.
3. Clinical Trials and FDA Approval
To address the skepticism surrounding Botox as a migraine treatment, several clinical trials were conducted to evaluate its efficacy. These trials involved injecting Botox into specific areas of the head and neck muscles associated with migraines. The results were promising, demonstrating a significant reduction in the frequency and intensity of migraines in participants.
Based on these positive findings, the FDA approved Botox for the treatment of chronic migraines in 2010. This marked a turning point in the acceptance and recognition of Botox as a legitimate medical intervention for migraine prevention.
4. Evolving Insurance Coverage Policies
Following FDA approval, insurance coverage for Botox as a migraine treatment gradually expanded. However, coverage policies varied significantly among insurance providers, with some offering full coverage, while others imposed strict criteria for reimbursement. Many insurers required patients to meet specific criteria, such as a minimum number of headache days per month and documented treatment failures with other medications, before approving Botox coverage.
The lack of standardized coverage policies created confusion and frustration for patients seeking insurance reimbursement for Botox treatments. Many individuals had to navigate complex administrative processes and appeals to secure coverage, while others faced outright denials.
5. Advocacy and Legislative Efforts
Recognizing the need for improved access to Botox for migraine prevention, patient advocacy groups and medical professionals began lobbying for legislative changes. They argued that Botox was a cost-effective treatment option compared to other migraine medications, as it reduced the frequency of debilitating migraines and improved patients’ quality of life.
These advocacy efforts resulted in some states passing laws mandating insurance coverage for Botox as a migraine treatment. However, the extent of coverage and the specific criteria for eligibility still varied across states and insurance providers.
6. Recent Developments and Current State
In recent years, there has been a gradual increase in insurance coverage for Botox as a migraine prevention treatment. Insurance companies have recognized the growing body of evidence supporting its efficacy and cost-effectiveness. Some providers now offer more streamlined processes for obtaining prior authorization and reimbursement for Botox treatments.
However, challenges remain. Many patients still face barriers due to restrictive coverage policies, high out-of-pocket costs, or the need for extensive documentation to meet insurance requirements. Furthermore, insurance coverage for Botox may differ based on the type of insurance plan, such as private, Medicare, or Medicaid.
The historical context of ‘has anyone had success getting botox covered by insurance for migraine prevention’ reveals the initial skepticism and limited insurance coverage for botox as a migraine treatment. over time, as clinical trials demonstrated its efficacy and the fda approved its use, insurance coverage gradually expanded. advocacy efforts and legislative changes further improved access to botox for migraine prevention. however, challenges persist, and the current state of insurance coverage for botox varies among providers and requires patients to navigate complex processes.
FAQs
1. What is Botox and how does it work for migraine prevention?
Botox is a brand name for botulinum toxin, a neurotoxin produced by the bacterium Clostridium botulinum. It is commonly used for cosmetic purposes, but it has also been approved by the FDA for the prevention of chronic migraines. Botox works by blocking the release of certain chemicals involved in pain transmission, thereby reducing the frequency and severity of migraines.
2. Is Botox covered by insurance for migraine prevention?
Yes, Botox is covered by insurance for migraine prevention in some cases. However, coverage may vary depending on your insurance provider, policy, and medical necessity. It is important to check with your insurance company to understand the specific requirements and coverage details.
3. What criteria must be met for insurance coverage of Botox for migraine prevention?
Insurance coverage for Botox for migraine prevention typically requires meeting specific criteria. These criteria may include having a documented history of chronic migraines, trying and failing other preventive treatments, and receiving Botox injections from a qualified healthcare professional. Your healthcare provider can help determine if you meet the necessary criteria for insurance coverage.
4. How can I find out if my insurance covers Botox for migraine prevention?
To determine if your insurance covers Botox for migraine prevention, you should contact your insurance provider directly. Ask about the specific requirements and documentation needed for coverage. It is also advisable to consult with your healthcare provider, who can assist you in navigating the insurance process and provide any necessary medical documentation.
5. What costs can I expect if Botox for migraine prevention is covered by insurance?
If Botox for migraine prevention is covered by your insurance, you may still be responsible for certain costs. These costs can include deductibles, co-pays, and any portion of the treatment not covered by insurance. It is important to review your insurance policy and discuss the potential costs with your healthcare provider to understand your financial obligations.
6. What if my insurance denies coverage for Botox for migraine prevention?
If your insurance denies coverage for Botox for migraine prevention, there are several options you can explore. Firstly, you can appeal the denial by providing additional documentation or medical evidence supporting the medical necessity of Botox for your condition. You can also discuss alternative treatment options with your healthcare provider or explore patient assistance programs offered by the manufacturer of Botox.
7. Are there any side effects or risks associated with Botox for migraine prevention?
Like any medical treatment, Botox for migraine prevention carries some risks and potential side effects. Common side effects include temporary muscle weakness, neck pain, and headache. In rare cases, more serious side effects such as difficulty swallowing or breathing may occur. It is important to discuss the potential risks and side effects with your healthcare provider before starting Botox treatment.
8. How long does it take for Botox for migraine prevention to start working?
The effects of Botox for migraine prevention may not be immediate. It typically takes a few weeks for the treatment to start working. Some patients may experience a reduction in the frequency and severity of migraines within the first cycle of treatment, while others may require multiple treatment cycles to see significant improvement. Your healthcare provider can provide more information on what to expect in terms of timing and effectiveness.
9. How often do I need to receive Botox injections for migraine prevention?
Botox for migraine prevention is typically administered in a series of injections every 12 weeks. The treatment regimen may involve multiple injection sites on the head and neck. Your healthcare provider will determine the appropriate dosage and injection sites based on your individual needs and response to treatment.
10. Can Botox be used for migraine prevention in children?
Botox for migraine prevention is currently approved for use in adults aged 18 and older. Its safety and effectiveness in children have not been established, so it is not recommended for pediatric use. If your child suffers from migraines, it is important to consult with a pediatric neurologist or headache specialist to explore appropriate treatment options.
Concept 1: Botox for Migraine Prevention
Botox is a commonly known cosmetic treatment used to reduce wrinkles and fine lines. However, it is also approved by the FDA for the prevention of chronic migraines in adults. Migraines are severe headaches that can be accompanied by other symptoms like nausea, vomiting, and sensitivity to light and sound. Chronic migraines are defined as having headaches on 15 or more days per month, with at least 8 of those days being migraines.
When used for migraine prevention, Botox is injected into specific muscles in the head and neck. It works by blocking the release of certain chemicals that transmit pain signals. By preventing the activation of these pain pathways, Botox can help reduce the frequency and severity of migraines.
Concept 2: Insurance Coverage for Botox
Insurance coverage for Botox treatment for migraine prevention can vary depending on the insurance provider and the specific policy. In general, insurance companies are more likely to cover Botox for migraines if certain criteria are met.
One common requirement is that the patient must have a documented history of chronic migraines. This usually means keeping a headache diary or having medical records that show the frequency and severity of migraines over a certain period of time.
Insurance companies may also require that the patient has tried and failed other preventive treatments before considering Botox coverage. These treatments can include medications, lifestyle changes, and other non-invasive therapies.
Additionally, insurance companies may have their own specific guidelines regarding the number of migraines a patient must have per month to qualify for coverage, as well as the duration and intensity of the migraines.
Concept 3: Prior Authorization and Appeals Process
Getting insurance coverage for Botox for migraine prevention often involves a process called prior authorization. Prior authorization is a way for insurance companies to review and approve certain treatments before they are performed. It helps ensure that the treatment is medically necessary and meets the criteria set by the insurance company.
To obtain prior authorization for Botox, the patient’s healthcare provider will need to submit a request to the insurance company. This request typically includes medical records, documentation of the patient’s history of chronic migraines, and any previous treatments that have been tried.
The insurance company will then review the request and determine if the treatment meets their criteria for coverage. This process can take some time, and it is not uncommon for insurance companies to initially deny coverage for Botox.
If the request is denied, the patient and their healthcare provider have the option to appeal the decision. The appeals process involves providing additional documentation and evidence to support the medical necessity of the treatment. This can include letters from healthcare providers, medical studies, and other relevant information.
It’s important to note that the appeals process can be lengthy and may require persistence on the part of the patient and their healthcare provider. However, it can sometimes result in a successful overturning of the initial denial and approval of insurance coverage for Botox.
Overall, while insurance coverage for Botox for migraine prevention can be challenging to obtain, it is possible with the right documentation and persistence. It’s important for patients to work closely with their healthcare providers and insurance companies to navigate the process and advocate for their treatment needs.
1. Understand your insurance coverage
Before considering Botox as a treatment option for migraine prevention, it is crucial to understand your insurance coverage. Contact your insurance provider and inquire about their policies regarding Botox for migraine treatment. Ask about any specific requirements, such as prior authorization or documentation from a healthcare professional. Understanding your coverage will help you navigate the process more effectively.
2. Consult with a healthcare professional
Seek advice from a healthcare professional who specializes in migraine treatment. They can assess your condition, discuss the potential benefits of Botox, and guide you through the insurance process. A healthcare professional’s expertise will be invaluable in determining if Botox is a suitable option for your migraine prevention and in providing the necessary documentation for insurance coverage.
3. Keep a migraine diary
Maintaining a detailed migraine diary can provide valuable insights into the frequency, duration, and severity of your migraines. This information can support your case for insurance coverage by demonstrating the impact migraines have on your daily life. Include details such as triggers, symptoms, medication usage, and any attempts at alternative treatments.
4. Gather supporting medical records
To strengthen your insurance claim, gather all relevant medical records related to your migraines. This may include previous treatment plans, medication history, and any failed attempts at other preventive measures. These records can help substantiate the medical necessity of Botox as a migraine prevention option.
5. Research your insurance company’s medical policy
Insurance companies often have specific medical policies outlining their coverage criteria for Botox as a migraine treatment. Research your insurance company’s policy to understand the requirements they have set. This information will help you tailor your approach and ensure you meet their criteria when submitting your claim.
6. Document failed alternative treatments
Many insurance companies require documentation of failed attempts at alternative migraine treatments before approving Botox coverage. Keep a record of any non-Botox treatments you have tried, including medications, lifestyle changes, or other interventions. This documentation will demonstrate your commitment to finding an effective solution and support your case for Botox coverage.
7. Follow the insurance company’s submission guidelines
Carefully review your insurance company’s submission guidelines to ensure you provide all necessary information and documentation. Missing or incomplete information can lead to delays or denials. Pay attention to specific requirements such as forms, supporting documents, and any additional information they may request.
8. Be persistent and advocate for yourself
Dealing with insurance can be a challenging process, but persistence is key. If your initial claim is denied, don’t give up. Follow up with your insurance company, provide any additional information they may require, and appeal the decision if necessary. Advocate for yourself and your health by being proactive and assertive throughout the process.
9. Consider seeking assistance from a patient advocacy organization
Patient advocacy organizations can provide valuable support and guidance when dealing with insurance companies. They are often well-versed in the insurance process and can offer resources, advice, and assistance with appeals. Reach out to organizations specializing in migraine advocacy for additional support.
10. Stay informed about updates in insurance coverage
Insurance coverage policies can change over time. Stay informed about any updates or changes in your insurance company’s coverage for Botox as a migraine treatment. Regularly check their website, contact customer service, or consult with your healthcare professional to ensure you are aware of any modifications that may affect your coverage.
Remember, navigating the insurance process for Botox as a migraine prevention treatment can be complex, but with the right information and approach, it is possible to increase your chances of success. Stay informed, be proactive, and advocate for yourself to improve your chances of obtaining insurance coverage for Botox as a migraine prevention option.
Common Misconceptions about Getting Botox Covered by Insurance for Migraine Prevention
Misconception 1: Botox is covered by insurance for all migraine sufferers
One common misconception about getting Botox covered by insurance for migraine prevention is that it is automatically covered for all migraine sufferers. However, this is not the case. While Botox has been approved by the U.S. Food and Drug Administration (FDA) for the prevention of chronic migraines, insurance coverage for this treatment can vary depending on several factors.
Insurance companies typically have specific criteria that must be met before they will approve coverage for Botox injections. These criteria may include a documented history of chronic migraines, failed attempts at other preventive medications, and a certain frequency and severity of migraines. Each insurance provider may have its own set of requirements, so it is important to check with your specific insurance company to understand their coverage policies.
It is also worth noting that even if a patient meets the criteria for insurance coverage, there may still be limitations or restrictions on the number of Botox treatments covered per year. Some insurance plans may only cover a certain number of treatments within a specified time period, while others may require additional documentation or pre-authorization for each treatment.
Misconception 2: Botox is a guaranteed solution for migraine prevention
Another misconception is that Botox is a guaranteed solution for migraine prevention. While Botox has shown to be effective for many migraine sufferers, it is not a one-size-fits-all treatment and may not work for everyone.
According to clinical studies, Botox has been found to reduce the frequency and severity of migraines in some individuals. However, the response to Botox can vary from person to person. Some patients may experience a significant reduction in migraines, while others may see only a partial improvement or no improvement at all.
It is important to have realistic expectations when considering Botox for migraine prevention. It may take several treatment sessions before the full effects of Botox are realized, and some patients may require ongoing treatments to maintain the benefits. It is always recommended to consult with a healthcare professional to determine if Botox is a suitable treatment option for your specific condition.
Misconception 3: Botox for migraine prevention is only for cosmetic purposes
A common misconception about Botox for migraine prevention is that it is solely a cosmetic treatment and not medically necessary. While Botox is commonly associated with its cosmetic use for reducing wrinkles, it has also been approved by the FDA for the prevention of chronic migraines.
Chronic migraines are defined as having headaches on 15 or more days per month, with at least 8 of those being migraines. Botox works by blocking the release of certain chemicals involved in pain transmission, which can help reduce the frequency and severity of migraines.
Insurance coverage for Botox injections for migraine prevention recognizes the medical necessity of this treatment option. However, it is important to note that insurance companies may still require documentation and evidence of a patient’s chronic migraine condition before approving coverage.
It is also worth mentioning that Botox for migraine prevention is administered differently than cosmetic Botox injections. The dosages and injection sites for migraine prevention are specific to targeting the muscles and nerves associated with migraines, rather than targeting facial wrinkles.
Understanding the common misconceptions about getting Botox covered by insurance for migraine prevention is crucial for individuals considering this treatment option. It is important to recognize that insurance coverage for Botox can vary depending on individual insurance plans and their specific criteria. Additionally, while Botox has shown effectiveness for many migraine sufferers, it is not a guaranteed solution for everyone. Lastly, Botox for migraine prevention is a medically necessary treatment recognized by insurance companies, and it is not solely for cosmetic purposes. Consulting with a healthcare professional and working closely with insurance providers can help navigate the coverage process and determine if Botox is a suitable treatment option for migraine prevention.
In conclusion, obtaining insurance coverage for Botox as a treatment for migraine prevention can be a challenging and complex process. While some individuals have reported success in getting their insurance to cover the cost, many others have faced numerous obstacles and denials. The key factors that contribute to insurance coverage include having a documented history of chronic migraines, trying and failing multiple other treatments, and receiving the injections from a qualified healthcare professional. It is important for patients to be proactive in advocating for themselves, providing thorough documentation, and appealing any denials.
Furthermore, the specific insurance provider and policy can greatly impact the likelihood of coverage. Some insurance companies have strict criteria and may require prior authorization or a pre-determined number of failed treatments before approving Botox. Additionally, the cost and frequency of treatments can vary, with some insurance plans covering only a portion of the expenses. It is crucial for patients to thoroughly review their insurance policy and consult with their healthcare provider to understand the potential costs and coverage limitations.
While navigating the insurance process for Botox coverage may be daunting, it is not impossible. By understanding the requirements, gathering necessary documentation, and persistently advocating for coverage, individuals suffering from chronic migraines can increase their chances of success. It is also important to stay informed about any changes in insurance policies and guidelines, as coverage criteria may evolve over time. Ultimately, with patience and perseverance, individuals may be able to access the benefits of Botox as a preventive treatment for migraines.